"I implore people to check out hospices - if you've got the choice to use them, then use them. It's not all doom and gloom."
- Jonnie Irwin, lung cancer patient
About 1.7 million people die of lung cancer each year (1). It accounts for about 1/5 of all cancer-related deaths worldwide. Palliative care is medical care aimed at improving the quality of life of seriously ill patients. While it does not have the goal of providing curative treatment in all cases, its principle lies in improving quality of life and providing comfort. The holistic nature of palliative care also ensures that it is not just physical symptoms that are addressed, but the psychosocial aspect of disease as well.
Previous studies have been done to determine the actual benefits of palliative care. In lung cancer, palliative care improves patient and caregiver outcomes and is also associated with fewer medical interventions near the end of life (2). Healthcare costs and utilization are also improved (3). Palliative care is associated with decreased cost, and as the clinical and economic benefits of palliative care for metastatic cancer patients become evident, more patients are seeking treatment (4).
What specific benefits does palliative care provide for cancer patients? Research has shown that there are benefits for the patients in the following aspects: symptom management, knowledge of the disease, and holistic approach.
Some of the common physical manifestations of cancer include pain, anorexia, cachexia, fatigue, nausea, constipation, dyspnea, and malignant bowel obstructions. These physical symptoms as well as the related spiritual and psychosocial distress during a patient's treatment course are routinely addressed by physicians. Recent clinical studies that measure patient feedback and patient-reported outcomes have shown an added clinical benefit, empowering patients to participate in decision-making and allowing for earlier detection of symptom recurrence. It has been demonstrated that patients initiating chemotherapy who are trained to notify their healthcare teams with interval symptoms have a higher quality of life and improved overall survival compared with patients who receive usual care (5).
In comparison to patients who never participated in or only had minimal conversations about disease outcomes with their physicians, patients involved in treatment planning had higher illness understanding scores and better insight into the terminal nature of cancers. In addition, conveying information with compassion correlates with patients' satisfaction with care, as content presented in a more optimistic manner is often associated with higher levels of perceived physician expertise.
It is now common knowledge that systemic chemotherapy without a clear benefit for patients at the end-of-life results in excessively toxic outcomes. Delayed referral to hospice and palliative care may not improve survival, but it may improve patient outcomes in terms of quality of life (6). Given the proven value of palliative care in oncology for symptom management, quality of life, and prognostic understanding of terminal illnesses, there has been growing evidence in the last decade to support the early provision of palliative care for cancer patients in general, not just for lung cancer.
The median survival of patients randomized to early palliative care was 11.6 months, whereas the median survival of patients receiving standard oncologic care alone was 8.9 months (p = 0.02). Patients assigned to early palliative care also received less aggressive cancer-directed care, including chemotherapy, at the end of life (7). Thus, not only does palliative care prolong survival in some cases, but it also results in the removal of unnecessary treatment modalities that may increase management costs. While some may view referral to palliative care as an added expense, studies tend to prove otherwise, as the benefits far outweigh the increased initial cost of palliative care referral.
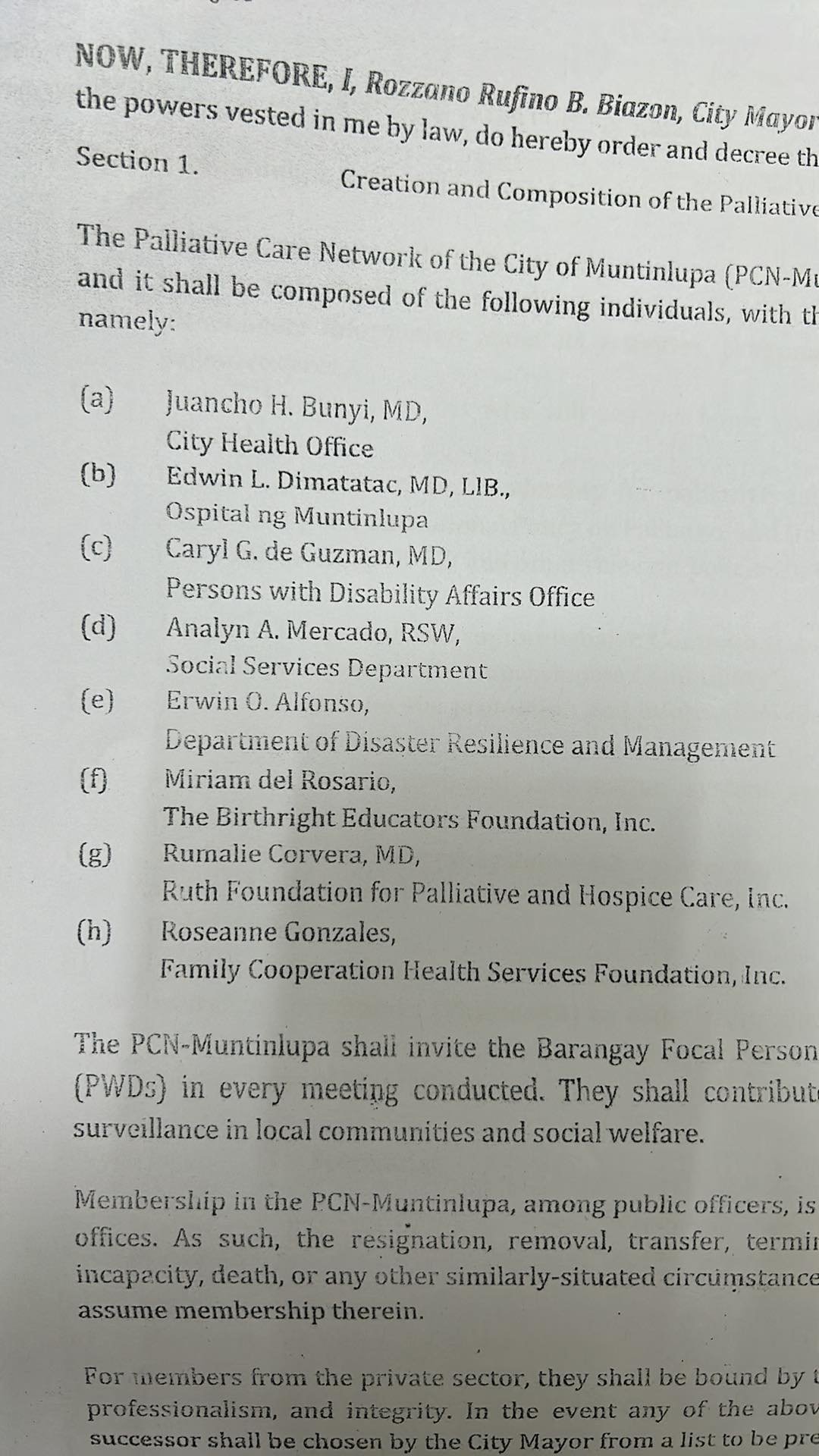
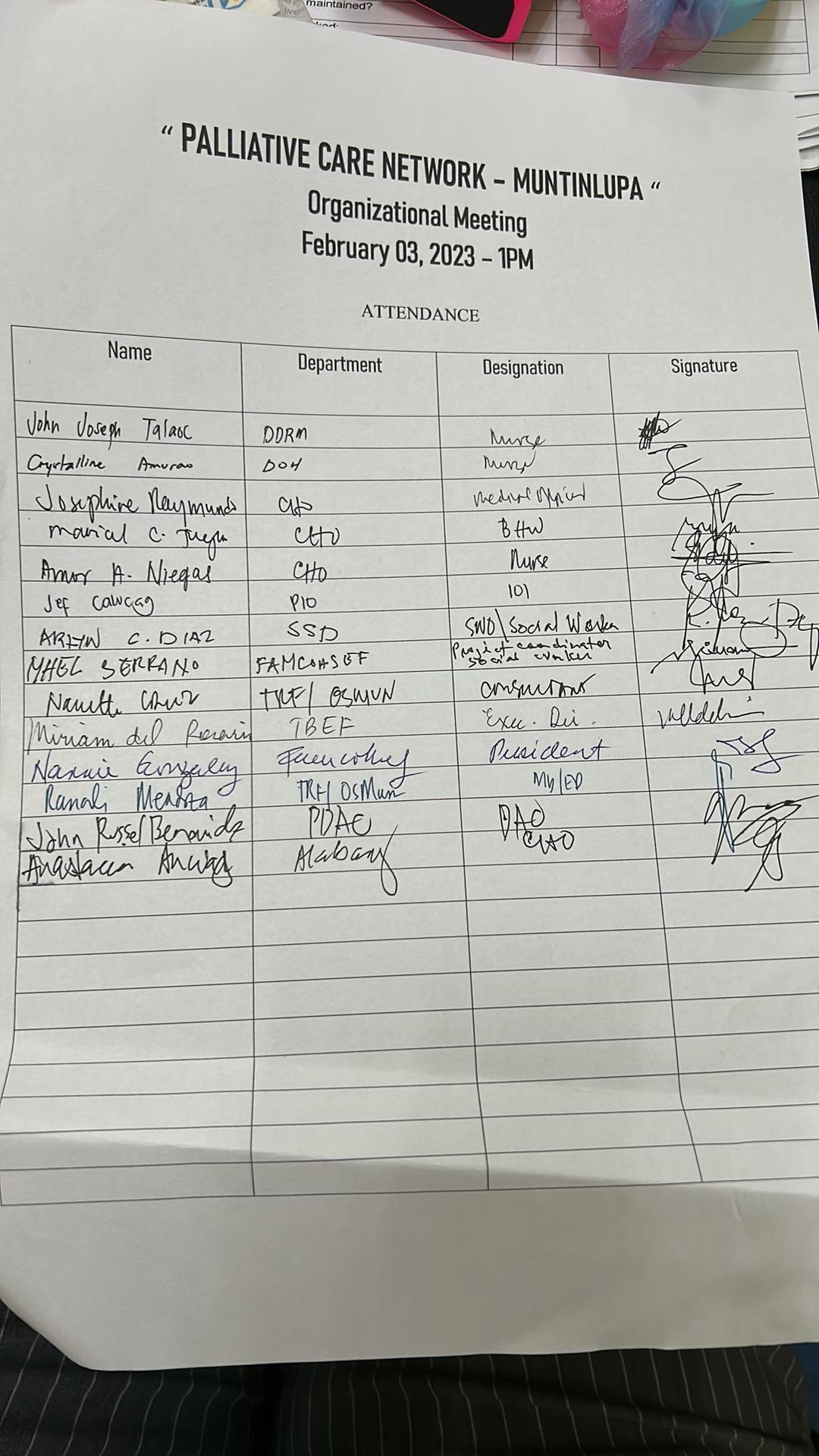
With the advent of Universal Health Care, and in conjunction with Republic Act 11036 or the Mental Health Act for providing mental health facilities in the community, palliative care must also be provided on a larger scale. The physical and psychosocial aspects of illness could be better addressed with early referral and management. It could mean the difference in terms of overall health outcomes.
REFERENCES
1. Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2016;388:1459–544.
2. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2010;363:733–42.
3. Lubitz JD, Riley GF. Trends in Medicare payments in the last year of life. N Engl J Med. 1993;328(15):1092–6.
4. Huo J, Hong YR, Turner K, Bian J, Grewal R, Wilkie DJ. Utilization pattern and service settings of palliative care for patients with metastatic non-small cell lung cancer. Cancer. 2019;125(24):4481–9.
5. Basch E, Deal A M, Kris M G et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. 2016;34(06):557–565.